
Classification of Technique:
1. Vacuum tube technique. (Tube excited by
Oudin or Tesla currents.)
2. Fulguration.
3. Constitutional (auto-condensation and auto-conduction).
4. Diathermy. (Direct D’Arsonval; electro-coagulation;
thermo-penetration.)
1. VACUUM TUBE TECHNIQUE.
This involves the use of the tubes by direct contact,
by effleuve (fine spray) and by actual sparks, from the mildest form to
the sharp caustic forms. It may be classified otherwise according
to its use as in (a) skin diseases, ulcers, inflammatory processes, etc.;
(b) relief of pain, as in neuralgias, etc.; (c) orificial application.
Vacuum tubes are employed where an essentially local effect
is desired.
Lubrication of Tubes. Any of the lubricating
jellies, unguents or cerates may be employed on tubes used within the urethra,
vagina or rectum.
Vaseline answers very well, for, although it is a non-conductor
of ordinary electricity, the thin coating required on these tubes is absolutely
no bar to high frequency currents.
Cautions. 1. As stated in Chapter V.,
high frequency currents are capable of producing annoying but not ordinarily
serious surface burns. These effects are especially quick to appear
when mucous surfaces are treated, as in rectal, vaginal, urethral or nasal
applications, and also in treating diseased areas about the lips.
On this account the application should be relatively short and mild if
a spark is employed in treating within the various orifices. Make
it a general rule never to allow a vacuum tube to remain in contact with
a mucous membrane for more than seven minutes at one treatment.
2. When the current is one of relatively high amperage,
the spark will set fire to any easily inflammable material. This
may be illustrated by lighting the gas with the spark, as previously referred
to. On this account care must be exercised in treating certain areas.
3. When introducing glass sounds into the male urethra
great care must be exercised not to use any undue force and thereby break
off the glass tube within the canal. These tubes are made of strong
glass, but may be broken by unusual pressure, or by a sudden jerk.
If difficult of introduction it is better to pass steel sounds first to
a size larger than the glass sound, as suggested in Chapter VII under Urethral
Technique.
Care of Vacuum Tubes. Asepsis. Although the
spark or effleuve from the vacuum tube is germicidal in character, still
it is the duty of the physician to use the utmost care and cleanliness
in employing it in order to guard against any possibility of spreading
infection from one patient to another.
In other words he would better follow some definite system
of sterilizing and disinfecting the tubes, and the nearer this is to surgical
asepsis the better.
Wiping off the tubes on a cloth or towel or simply rinsing
in water is not enough.
Apply the test to yourself. How would you like to
be treated with a tube that had been used in contact with a specific disease
and which had received no further cleaning than mere dipping in water and
then being wiped off with a towel that had already done similar service
an indefinite number of times?
Let your technique be so careful and conscientious that you
need never blame yourself for spreading contagion or infection of any kind.
This is a subject that I have not seen mentioned in any
treatises on high frequency currents.
Do not use the same tube for specific and non-specific
orificial cases. This alone will do much toward lessening the danger
of infection.
As these tubes bear heating, they may be sterilized by
boiling, just as surgical instruments are sterilized.
This, however, is not necessary, as immersion in strong
antiseptic solutions will be sufficient.
A tube that is to be used in contact with a mucous membrane,
such, for instance, as a vaginal or urethral electrode, should be immersed
in pure carbolic acid or in pure crethol, benetol or lysol, before again
using, if it has been in contact with the discharge from a specific disease.
In cases such as acne, psoriasis, eczema, neuralgia, non-specific
diseases of the urethra, rectum or vagina, etc., it will suffice if the
tube is immersed for a few moments, or kept permanently, when not in use,
in a strong solution of any one of the three antiseptics mentioned in the
preceding paragraph.
For this purpose a glass jar, large enough to take in
the various electrodes, should be filled with a twenty percent solution
of carbolic acid (a five per cent solution is not enough); or as its equivalent,
one of crethol, benetol or lysol containing a tablespoonful of either to
the pint of water.
An ideal way would be to have two jars, one containing
the full strength antiseptic, for the tubes employed in infectious cases,
and the other for those used in non-contagious diseases.
Personally I prefer crethol or lysol to carbolic acid,
because equally satisfactory and not caustic if any of the full strength
liquid accidentally comes in contact with the operator’s hands.
If the tubes are immersed in the pure antiseptic they
should be thoroughly rinsed in alcohol and water, or in water alone before
using. From the weaker solutions, water alone is necessary, but in
both cases hot water is preferable.
The conveniences of most of our modern office buildings
make the technique of sterilizing the tubes a simple one in the large cities,
but in smaller towns the physician will find it somewhat more of a task.
In the absence of large jars to keep the two solutions
in, with the tubes constantly immersed, wide mouthed bottles may be employed
for use before and after each treatment.
By sterilizing in this manner both before and after, the
tube not only receives a double sterilization, but also if it has been
taken care of immediately after use, if such a thing should happen that
it should be used again without remembering about sterilizing it, the danger
would be slight, and furthermore the tube is easier sterilized immediately
after using, than it is when the secretions or discharges have dried upon
it.
I have spoken of using the same care that you would with
a surgical instrument, although the danger with these tubes is not as great
as with surgical instruments for several reasons. In the first place,
they are not employed ordinarily in a fresh wound: secondly, the danger
is in carrying infection from one patient to another and not the additional
danger which accompanies a surgical operation, of infecting the wound from
the individual as well, and finally, in the majority of the cases treated
there is practically no serious danger of infection.
If one had a sufficient number of tubes it would be desirable
to keep an individual tube for each patient, which was used for no other.
Immersion in the weaker solutions referred to above and rinsing, or even
ordinary cleanliness would be sufficient; but at the close of the course
of treatments, before the tube was used for another case it then should
receive vigorous and thorough sterilization, in proportion to the danger
of infection involved in the case.
The sterilizer shown in Fig. 28 is an excellent one.
A basin of formalin solution keeps the tubes always sterile.
Some of my readers may think I am devoting too much space
to this subject, but it is an important one, and my early surgical training
has made me a “crank” on this point, and really, could you ever excuse
yourself if through your carelessness you spread, say a specific infection,
even in one single instance.
Measuring Dosage. One problem that confronts
the physician who is beginning to use the high frequency is a method of
measuring dosage. There is no meter which will measure the output
of the vacuum electrode, or in other words the unipolar current.
For auto-condensation and for diathermy the hot-wire meter is used and
proves relatively satisfactory. For the vacuum tube, in order to
convey an idea that would apply, no matter what size or make of apparatus
might be employed, I have made use of the length of spark which it is possible
to draw from the vacuum tube as a simple method of giving some idea of
the strength of current employed. This is a very crude method, and
open to some serious objections, but will answer the purpose in a general
way and convey a more intelligent idea than any method other than a meter.
With a definite amount of current passing through the
apparatus, there is a positive point near the tube that represents its
utmost sparking distance, that is, the longest spark that can be drawn
from that tube, and this will remain constant as long as the current is
constant – lessening the current shortens the spark; increasing it, lengthens
it. Therefore, if I say I employ for skin diseases a tube capable
of yielding a one-quarter inch or one-half inch spark, I give to the physician
a definite idea of the amount of current I would employ in the tube.
This does not take into consideration the sharpness of
the spark, which must be adjusted in accordance with individual susceptibility
and the type of machine used.
With the Tesla type of apparatus and particularly with
small machines, the spark is apt to be sharper in proportion, and is designated
frequently as a “hot” spark. With these outfits it is often impossible
to employ a spark more than a quarter of an inch in length. With
other types, a longer spark will be tolerated, and with the Oudin type
of apparatus we have what may be called a “cold” spark, and frequently
one three-quarters or an inch long may be more easily borne than a quarter-inch
“hot” spark. The cold spark is dehydratory and the hot spark caustic.
In interpreting my suggestions for dosage in Chapter VIII, these facts
should be taken into consideration. Ordinarily if the dose is given
one-fourth to one-half inch the first would be for the “hot” and the second
for the “cold” spark.
The Eberhart. Author’s Unit of Measurement for
Auto-Condensation. For a long time both physicians and manufacturers
have felt the need of a standard unit for measuring auto-condensation;
one that would fairly represent the auto-condensation output of any type
of machine. I believe I have solved this problem, and have a standard
of measurement that will prove acceptable to the manufacturers of any form
of apparatus. It will be found convenient for the manufacturer to
state with the directions for auto-condensation that the output of the
machine is so many Eberharts per minute to each 100 milliamperes registered
on the hot-wire meter. In this way with the dosage given as a certain
number of Eberharts, it is easy to note by the meter how many Eberharts
are passing per minute and by noting how many times this number will go
in the total dose stated the number of minutes required for the treatment
is ascertained.
There are three essential elements entering into auto-condensation.
First, the pressure or potential (voltage); second, the rate or meter reading
(amperage); and third, the time. When the voltage is high the amperage
is correspondingly low, and vice versa. In a general way the effectiveness
of any machine for auto-condensation may be expressed in terms representing
the product of the voltage and the meter reading (equivalent of amperage).
Thus 50,000 volts at 500 is the same as 25,000 volts at 1,000; each representing
an auto-condensation effectiveness of 25,000,000.
My unit of measurement for auto-condensation is based
on the passage of 1,000 volts at a rate of 100 milliamperes in one minute
of time. This unit I call the Eberhart and abbreviate it E.
We have two types of apparatus for auto-condensation,
the one high voltage and comparatively low amperage; the other low voltage
and high amperage. In a general way I assume that the first represents
a current of about 50,000 volts delivered at a rate of 350 to 500 milliamperes
as shown on a hot-wire meter. The second averages 25,000 volts, potential,
and is ordinarily delivered at a rate averaging 750 to 1,200; 1,000 being
a frequent rate. Applying our unit it will be seen that 50,000 volts
equal 50 E. For each 100 milliamperes meter reading, and if the meter read
500, there would be delivered 5 times 50 or 250 E. For each minute of time,
and this would give 2,500 E in a ten-minute treatment. With the other
machine 25,000 volts equal 25 E. Per 100, and with meter at 1,000 would
give 10 times 25 E. Or 250 E. Per minute, or 2,5000 E. Would require a
ten-minute treatment.
The manufacturer may state the voltage of his machine,
if desired, but the simpler way is to give the number of Eberharts to each
100 milliamperes meter reading. He should also state the average
meter reading at which the apparatus is to be operated. If he states
the voltage, to compute a required dose, multiply the meter reading by
the number of thousand volts, and divide this product by 100. This
is the number of Eberhart units being given per minute, and by dividing
the dose as given in Eberharts by this, we have the number of minutes required.
Going back to our previous example: to give 2,500 E. auto-condensation
on a machine of 50,000 volts with enough current passing to raise meter
to 500, multiply number of thousand volts, 50 by meter reading 500, and
product is 25,000. Divide by 100, which is done by cutting off two
ciphers, and we have 250, which is the number of Eberharts per minute–250
goes into 2,500 ten times, therefore it takes ten minutes to give the required
dose of 2,500 E.
It will be seen that it would be much simpler if the manufacturer
stated with this machine that the auto-condensation output was 50 Eberharts
per minute for each 100 milliamperes registered by the meter. Then
if the dose to be given is 2,500 E. And the meter registers 500, or five
times the 100 rate, it is easy to figure then that 500 is five times 50
or 250 E., and this goes in 2,500 ten times, therefore it takes ten minutes
to give that amount.
With the other type of machine we will say that the output
is 25 E. Per minute per 100 milliamperes; but this machine will ordinarily
be operated at about 1,000 milliamperes, or ten times 100, therefore it
is also delivering ten times 25 E. Or 250 E. per minute, and it will also
take ten minutes to give 2,500 E. In Chapter VIII the dosage of auto-condensation
will be stated in Eberharts.
It is well to remember that there is essentially no danger
in auto-condensation and therefore no over-dose, so that the dosage stated
may be greatly increased if results are not obtained.
The only cases in which caution is necessary, are those
where a patient is carrying a high temperature or where the pulse pressure
is 20 or lower.
Preparation of Patient. When the surface
of the body is to be treated, the question of removing the clothing arises.
If no spark is desired, the electrode must be in contact with the skin,
and any clothing covering the part must be removed.
All metal, such as chains, corset-steels, wire hairpins,
etc., with which the tube comes in contact or within sparking distance
of, will be charged with the current and give rise to sharp and disagreeable
sensations. If they cannot be avoided they should be removed.
Applications to the body, calling for a mild spark, may
be given through thin underclothing, or the patient stripped and covered
with a sheet, through which the spark is employed.
Aside from the reason spoken of above (chains, etc.),
when a sharp spark is required there is no especial need of removing the
clothing, in fact, a definite thickness insures a definite length of spark.
When the tube sticks on the skin, dust on talcum powder
or lay over the surface a very thin cloth, such as a handkerchief.
In vaginal treatments no disrobing is necessary.
General Technique in Skin Diseases and Surface Lesions.
In applying the high frequency spark over the surface of the body, as in
acne, eczema, etc., I employ a current of sufficient strength to produce
a spark one-quarter to three-quarters of an inch in length. The discharge
from the smaller Tesla coils is relatively sharper than from the resonator
or larger Tesla outfits, and a shorter spark is used, as the patient cannot
tolerate quite as much current in these instances. With a vacuum
electrode capable of delivering a spark of the length given, I do not try
to make use of the full length spark, but keep the tube in light contact
with the skin, thus giving a sufficient intensity of current, but avoiding
the pain that would result if the tube were held at full sparking distance
from the surface. The tube is passed rapidly back and forth over
the area treated, and this will be accomplished in the easiest manner by
holding the tube handle lightly with the fingers, with the thumb extended
along the handle. A side to side motion with the wrist will soon
become a matter of habit to the operator and the tube will pass lightly
over the surface without any sudden jerks or elevations to cause annoying
sparks.

If the skin is moist and the tube sticks, it may be dusted
with talcum or other dusting powder to obviate this difficulty. Another
method is to place a thin cloth over the surface, which will enable the
tube to be used smoothly and at the same time does not remove it far enough
from the surface to make an unpleasant spark.
Where itching is marked, the tube is raised from the skin
and as sharp a spark applied as the patient will tolerate for a short period
of time. This quickly relieves the itching and also quickly produces
the characteristic reaction of the current (hyperemia, etc.).
In treating epithelioma, lupus and any chronic ulcers,
a spark is employed in the same manner, that is, as sharp as the patient
can stand, but not for a long period, say from two to three up to occasionally
five minutes. Unless cauterization is sought, the tube should be
kept moving rapidly over the surface and not allowed to expend its full
effect steadily over any minute area. At the present time fulguration
(caustic) would be employed more frequently for epithelioma and lupus.
Technique for Relief of Pain. In congestive
headaches, neuralgias and other painful conditions, the beneficial action
of the high frequency current seems to be largely the result of counter-irritation.
Therefore, it makes very little difference whether a sharp spark is used
with the rapidly moving tube at full sparking distance, or whether with
the same intensity of current, the tube is kept in contact with the skin.
It depends upon the sensitiveness of the patient and also upon the location
of the area treated. A long sharp spark occasionally exerts a slight
caustic effect, and the surface will be covered with tiny blebs, which
are followed by minute scabs, making the skin sore and uncomfortable.
Unless the case to be treated is a severe one, it is not permissible to
push the treatment to this degree.
Cauterization. If a hot spark is held steadily
over the spot for from thirty seconds, up to two or three minutes, varying
with the patient, it will have a cauterizing effect. The reaction
is severe and the destruction of the tissue may be carried to a marked
degree. Such applications have been used in the treatment of warts,
moles, etc.
I have treated epitheliomas in this manner and have had
them separate from the surrounding tissue and peel out as smoothly as if
cut out with a die. It is too severe a measure, however, for the
average case. Fulguration involves the same principles, and is preferable.
The spark is derived from a metal point and anesthesia may be employed
if desired. The technique of this will be considered in another section.
Orificial Technique. The technique of the
application to the orifices of the body involves the use of tubes suited
to the various areas, and also involves the question of sterilization and
lubrication. In these cases the tube is in contact with the mucous
membrane and there is no sensation to the treatment except usually that
of warmth. There is in these cases greater danger of producing burns,
and the tube should seldom be left in contact for a longer period than
seven minutes at any single treatment. (See the section on vacuum
tube burns in Chapter V.) The technique is so peculiarly that of
the special organ involved that it will be given under its appropriate
heading in Chapter VII. It is desirable to remember that tubes should
always be inserted before the current is turned on, and the latter turned
off again before the tube is removed, thus avoiding all pain and shock
to the patient.
Cataphoresis. For cataphoresis a special
electrode is employed. See Fig. 29. The substance to be carried
into the tissues is in solution, and cotton gauze or felt wet in the solution
is placed in the depression on the face of the tube when the latter is
placed in contact with the desired area and the current passes for from
five to ten minutes or more as required. I caution against the use
of solutions containing alcohol or other inflammable substance because
of the danger of setting same afire with the current.

In one form an insulating ring prevents loss of current
and is a great improvement on the older style of tube.
See Chapter XII for special electrodes used by dentists.
Although strong claims have been made concerning the value
of high frequency currents for the purpose of carrying substances into
the tissues, I believe they are so far inferior to the galvanic current
for use for these purposes that they are entitled to comparatively little
consideration.
The principle upon which cataphoresis depends is the separating
of the particles (ions) composing the fluid by reason of the attraction
possessed for them by the poles of the battery; thus all positive elements
remain at or are drawn through the tissues toward the negative pole, and
vice-versa. Now, in using high frequency currents, which are alternating,
the attraction would be first in one direction and then in the other and
as a result practically nothing would be accomplished.
The claim is made that the high frequency current drives
substances into the tissues by “molecular bombardment.” I maintain,
however, that the cataphoric action of the high frequency current is too
feeble to commend it for general use, for which purpose nothing takes the
place of the galvanic current.
The use of dental electrodes for cataphoric purposes has
given good results. See Chapter X. It is really an electrical
diffusion, rather than true cataphoresis.
Bi-polar Tesla Technique. Ordinarily the
vacuum tube is attached to one pole of the Tesla outfit. In some
coils the sharpness of the spark is regulated by drawing off a certain
amount of the current from the active pole by bringing the sparking rod
near it, thus lessening the available current.
If it is desired to intensify the action of the Tesla
coil, the indifferent pole should be attached to the patient or grounded
by connecting to a gas or water pipe.
Selection of Most Suitable Form to Use. Where
a local effect is more essential, vacuum tubes, metal electrodes, etc.,
are employed, but if a systemic or constitutional effect is desired, auto-condensation
is to be selected, or the diathermic treatment may be used.
2. FULGURATION.
Fulguration. A long sharp spark for escharotic
or destructive purposes was employed for a long time by high frequency
operators, but the use of a metal electrode devised by Keating-Hart for
this purpose, which he termed fulguration, gave an unusual impetus to the
method.
Fulguration as employed at the present time may be considered
under two forms: 1. Caustic or hot fulguration, employed with D’Arsonval
or Tesla apparatus, and giving a hot, caustic or cauterizing spark.
The D’Arsonval fulguration is particularly suitable in orificial work,
such as papilloma of the bladder, etc. The Tesla is especially advantageous
in surface work, such as moles, warts and other superficial growths.
2. Dehydratory or cold fulguration, employed
with Oudin apparatus. The destruction of tissue is through a drying
process and there is no sloughing. There is essentially no pain,
but its range is necessarily limited.
Dr. W. F. Clark of Philadelphia employs a method of cold
fulguration with the static machine, to which he has applied the term dissication.


General Caustic Fulguration. The technique
which I employ for warts, moles and small growths is as follows:
The fulguration electrode is attached and the current
turned on gradually, while the length of spark from the metal point (Fig.
33), is tested by bringing the point nearly in contact with a piece of
metal, such as a coin. Without an anaesthetic it is impossible to
employ one more than one-thirty-second to one-eighth or occasionally three-sixteenths
of an inch in length. This spark is hot, and actually sears or burns
the tissue, as noted by the eye and usually by the odor.


It is not desirable to keep this spark in steady contact,
as it is too painful, but if the point is touched to the surface and quickly
brought away beyond sparking distance, the patient is better able to stand
it, and by a series of rapid sparks produced by a tapping motion of the
point, thorough fulguration my be achieved without unbearable pain to the
patient. Ordinarily I pass around the margin of the growth first,
and then fulgurate the center. It should be done thoroughly, and
the growth will present a brown, burned appearance. There is seldom
any hemorrhage, but usually some serious oozing. A crust or scab
forms which separates in a week or ten days (average eight), leaving no
scar. It is well to bear in mind that if you do not get it all off
the first time you can fulgurate again, but if you remove too much you
cannot place it back again.
For more extensive work, local or general anaesthesia
is necessary.
It is fair to state that very satisfactory caustic (hot)
fulguration may be accomplished with small machines.
In papillomata of the bladder, fulguration has been particularly
valuable.
Fulguration of Papillomata of Bladder. The
hot or caustic fulguration may be employed, using wire insulated with rubber
tubing, or the D’Arsonval method, which is bi-polar, may be used, as follows:
One terminal of the apparatus is connected to the fulguration wire, which
is passed through the cystoscope, and the other terminal is connected to
an indifferent flat metallic electrode placed on the abdomen. The
fulguration wire or electrode consists of a steel wire insulated with pure
gutta-percha. As this wire is to be passed through the channel of
an ordinary catheterizing cystoscope, it should not be larger in gauge
than No. 6 French.
The patient is prepared with green soap and water and
bichlorid, and the bladder distended with water. After the cystoscope
is introduced, the tumor is brought in view and the fulguration wire passed
through the catheter channel of the cystoscope until the end of the wire
is in view. The wire is then plunged into the tumor and the current
turned on. (Before introducing the wire into the cystoscope, cut
the wire so that the insulation is flush with the end of the wire.)
Just as soon as the high frequency current is turned on, bubbles (presumably
hydrogen) are seen emanating from the tumor. If the tumor is small,
or the electrode has been placed near the top of the tumor, an immediate
blanching of the tumor is seen. This treatment can readily be carried
out under the guidance of the eye, providing the insulation of the fulguration
wire is intact; unless the insulation is intact, a short-circuit in the
cystoscope and subsequent burning out of the cystoscope lamp may result.
After allowing the current to pass into the tumor for
about twelve to fifteen seconds, the current is shut off, the fulguration
wire withdrawn and re-applied to another part of the tumor. In large
tumors, this procedure can be repeated until many different areas of the
tumor have been treated in one sitting. As long as five or six minutes
may be consumed in one sitting. Naturally, the duration of each treatment
will depend on the size of the tumor. For example, in one case, one
sitting consisting of three 12-second applications was enough to completely
destroy a small papilloma.
As long as the intra-vesical electrode remains in contact
with the tumor no pain is experienced by the patient. When working
near the base of the tumor, or if the electrode comes in contact with the
bladder-wall, the patient frequently complains of pain. So that during
the first fulgurations there is no pain, whereas, toward the end f the
treatment, while working near the bladder in treating the remaining tags,
the patient at times complains of pain. It is also necessary to consider
the pain incident to cystoscopy. This is variable in different persons,
so that some of the patients cannot tolerate long sessions as well as others.
The number of treatments or sittings, as previously stated, is determined
by the size of the tumor, some cases requiring as many as six sittings.
Attention is called to the burning off of the insulation
near the end of the fulguration wire. After the current has been
turned on and the treatment carried on for a little while, sometimes only
ten seconds, the insulation becomes soft, and falls off or burns off from
the end of the wire, so that it becomes necessary to withdraw the wire
and cut the end off squarely. Unless this is done, there is danger
of the bare wire causing a short-circuit in the cystoscope.
Usually when the high frequency current is applied the
tissues become white and shrivel up. Sometimes the tumor surface
appears dark, as though it were baked. Not infrequently after an
application a larger or smaller piece of the tumor adheres to the end of
the fulguration wire. At other times these small pieces may be passed
at the next urination, and often they are obtained from the wash water.
These are carefully saved and examined microscopically.
It is suggested that papillomata should be considered
malignant in all cases; that in all cases of long standing cystitis which
has persisted even in the presence of careful treatment, or with the history
of frequent relapses, papilloma should be suspected, and the diagnosis
confirmed or contradicted by cystoscopy. It is the consensus of opinion
that the fulguration method is followed by remarkable results, but as yet
sufficient time has not elapsed for us to make a definite statement as
to an absolute guarantee that this treatment will prevent recurrences.
(Abstracted from an original article,

“Fulguration Treatment of Bladder Tumors,” by Herman L. Kretschmer, M. D., of Chicago. Illinois Medical Journal, April, 1913.)
3. CONSTITUTIONAL (AUTO-CONDENSATION AND AUTO-CONDUCTION).
Auto-conduction. In auto-conduction the patient
is placed within a large solenoid or coil, constituting a cage. The
patient is not in contact with this cage at any point and the high frequency
currents in the patient’s body are produced by conduction.
The cages are of several types, some in perpendicular
form, and others in a horizontal position. In the latter the patient
is either placed on a board which slides into the cage, or the top of the
latter is hinged like the cover of a basket. Some of the perpendicular
forms are collapsible, others are fitted with a door, the patient standing
or sitting on a stool.
Small cages are also made into which the arm or leg may
be introduced, thus producing localized auto-conduction effects.
The dosage is the same as with auto-condensation.
Owing to an inherent objection on the part of the human
race to being incarcerated in a cage, even for a short time, this method
of treatment, although excellent in results, is used comparatively little
at the present time; furthermore, it has no advantage over auto-condensation.
Auto-condensation. In auto-condensation,
one of the terminals of the apparatus is attached to the metal forming
one plate of a condenser and the other to the patient, who becomes in this
manner the other condenser plate.

The patient is insulated from the metal plate by silk floss,
rubber, mica, glass, or other form of dielectric.
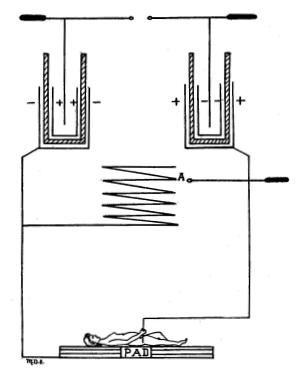
In Figure 36 is shown a cross-section of a plate condenser.
In Figure 37 the body of a woman is substituted for the upper plate, thus
showing the principle involved in auto-condensation.
Auto-condensation is administered by means of a couch
or pad designed for the purpose and may include the whole body or be constructed
to influence only a part of it.
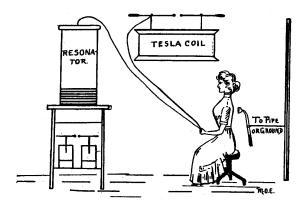
The original couch was in a form similar to that of a
Morris chair (Fig. 38), the plates of zinc being under the cushions on
back and seat, the cushions themselves being stuffed with silk floss or
with Spanish moss. The plates connect with one binding post of the
apparatus, and the other is connected to a rod from which wires run to
metal handles on each side, which are held by the patient, who receives
the charge whether one or both handles are grasped.
In that part of the circuit that is connected to the handles
a hot wire meter is placed to measure the dosage. No other form of
electrical treatment gives so high an amperage, except diathermy, the dose
running from 150 to 1,500 milliamperes, with occasional reports of the
use of even a stronger dose.
It is well to remember that there are two types of machines
used in producing auto-condensation. One has high voltage, but comparatively
low amperage, requires a cushion at least three inches thick and has great
penetration, so that a vacuum tube will light up within an area of several
feet surrounding the patient. With this type the average meter reading
to obtain satisfactory result is 350 to 500. It is seldom necessary
or desirable to secure a higher reading. Lower readings, 150 to 200,
would be used where it was desired to influence nutrition without particularly
lowering blood-pressure.
The other type machine has comparatively low voltage, but
high amperage. It may be used with a thin pad if desired. The
meter will read 750 to 1,000 on an average, and up to 1,200 or 1,500, according
to the potential of the apparatus. Auto-condensation is measured
in Eberharts, as stated in a preceding section in this chapter.

As long as the patient is in electrical contact with the
handles, that is, perfect contact, no sensation is felt except occasionally
a slight tingling or sensation of warmth. Sparks may be drawn from
the patient, and these may be quite painful. In type No. 1 a vacuum
tube held in operator’s hand will draw a spark from patient which is known
as one form of indirect spark. In general, a feeling of warmth pervades
the body after a few moments, and the temperature is shown by the clinical
thermometer to be from one-half to one degree higher than before the treatment.

The couch or cushion is connected to one terminal of the
apparatus, the patient to the other. The static machine with hyper-static
transformer does not give a sufficient amperage for the satisfactory operation
of a couch; neither does the average portable outfit, although the latter
has more amperage than the static machine. Both of these may be used
for charging small pads for restricted areas, and some types of the larger
portable coils I have found capable of operating a good-sized pad, if the
dielectric is thin.
In 1903 I designed the first portable body pad, which
folded together when not in use. It consisted essentially of the
top of the couch and was intended to save the space required for the latter.
About the same time Piffard produced a condenser pad for
the set of an ordinary chair (Fig 41)
It is a well-known fact that the thinner the di-electric
is, as long as it is a perfect di-electric, the greater the corresponding
charge that may be held on each layer of condenser. This caused me
to substitute flexible mica for the material used in the ordinary pad and
thus produce a portable auto-condensation pad only half an inch thick,
and capable of being slipped under the leather cushion of the ordinary
office treatment table, converting the latter into an auto-condensation
table. At the same time a much greater charge of electricity may
be condensed in the patient than with the thicker pads.
Pads less than three inches thick have been condemned
by the standardization committee of the American Electro-therapeutic Association,
therefore, at the present time I employ only the thick cushion.
Many ingenious operators construct their own chair or
couch, and from an article of mine on this subject in Popular Electricity,
November, 1909, I make a few excerpts:
“A glass slab, four or five feet in length, twenty inches
wide and about one inch thick, such as is used in a glass-topped operating
table, is fitted in a wooden frame and to the under surface is attached
a strip of zinc or of sheet lead 1/32 of an inch thick. This strip
should be about ten or twelve inches wide, so that when placed on the lower
surface of the glass it will leave a margin of about four or five inches
between the edge of the zinc and the edge of the glass. It should
extend lengthwise to within six inches of either end of the glass slab.
The zinc or lead plate is connected by an ordinary covered conducting wire
say, not smaller than No. 10 or 12, to one pole of the high frequency apparatus
and the patient connected by an ordinary metal electrode to the other pole.
The patient may be placed directly on the glass, but it is preferable to
place him on a thin cushion upon the glass, for sake of comfort.

“Another method is to take a wooden table long enough for
the patient to lie on and place underneath the table top a layer of plate
glass the full size of the top of the table with a strip of lead or zinc
attached to the under surface of this glass, always bearing in mind that
the essentials of an auto-condensation pad are to have a di-electric with
a layer of condenser below it, and the patient attached to the apparatus
to form the upper layer. Thus, an ordinary Morris chair or steamer-chair
may be used and a layer of lead or zinc fastened underneath the back and
seat of the chair, the two strips being fastened together with metallic
connections (chain or wire) and underneath the ordinary cushion of the
chair, four or five layers of rubber are placed to serve as the di-electric,
although the cushions themselves, if they remove the body beyond the sparking
distance of the charge on the zinc plate, would really make the air space
intervening serve as a di-electric. This is not as satisfactory as
when the layers of rubber are placed between. The patient then is
connected by the ordinary metallic hand electrode and conducting cord or
metallic handles may be fastened on the arms of the chair, the two connected
by a bifurcated conducting cord to the one pole, the zinc plates to the
other.
“Lastly, a pad may be constructed on the same plan as
the one which I have designed, using one or more layers of sheet mica large
enough to permit the body of the patient to rest on and making use of a
layer of condenser either lead or zinc underneath the mica, taking care
that it does not extend near enough to the edge of the mica to allow the
charge to leak over. On top of the mica place three or four layers
of felt or cover with leather as desired. Should the mica be insufficient
to prevent some sparking through, it may be obviated by placing another
thin cushion on top of this pad.”
The patient is placed on the couch or pad and connected
to the apparatus before the current is turned on, and then the current
turned off before the patient lets go of the handles, thus avoiding all
shock.
If the patient questions whether he is getting any current
or not a few sparks drawn from his body readily convinces him.
Another form of treatment which the patient feels to the
extent of strong muscular contractions may be made by introducing a spark-gap
into the patient’s circuit. This I describe in another section as
D’Arsonval surgings.
The value of auto-condensation depends upon its remarkable
effect upon general metabolism (see Chapter V). In nearly all cases
of hypertension the blood-pressure is lowered.
Auto-condensation treatments average ten to thirty minutes
in duration (2,500 to 7,500 Eberharts), and should be given daily, or six
times a week at first, in nearly all cases, gradually decreasing as improvement
takes place. Less than three treatments per week at the start are,
in my opinion, practically useless. Longer treatment may be given
if the physician desires.
Cautions. There is practically no danger
of an over-dose of auto-condensation, the only danger being in cases where
the patient has a high temperature that will be raised still higher, where
a small dose, if any, is given, and in case of a pulse pressure below 20.
See section Taking the Blood Pressure, and under Arterio-sclerosis, Chapter
VIII. In low pulse pressure there is danger of obliterating the pulse
by auto-condensation.
Author’s D’Arsonval Surgings. I have alluded
to the fact that placing a spark-gap in the patient’s circuit causes strong
muscular contractions. The similarity between this and static “surging”
caused me to apply the term of “D’Arsonval surging” to this form of treatment.
I first noticed it when adjusting the sliding rod on a
D’Arsonval-Oudin resonator. This rod enables the operator to balance
the current between the coarse solenoid and the resonator, or “tune” the
coil. Doing this with the patient on the auto-condensation couch
caused the latter to exclaim at the resulting muscular jerks.

I use a high-voltage, low-amperage type of machine with
a thick pad. Enough current is turned on to give a meter reading
of about 250 (125 E.). A vacuum electrode is held in the operator’s
hand and the length and strength of spark tested by touching the metal
handle which the patient is holding, before the tube is applied to the
patient’s body. The current is then raised or lowered to provide
a suitable intensity and length of spark, after which the electrode is
applied to the portion of the body to be treated. The spark is drawn
from the patient’s body, is disruptive in character, and is particularly
suitable for various skin diseases, having also the advantage of the patient’s
nutrition and general metabolism being benefitted by the auto-condensation
which accompanies it. In other words, it is both local and general
in its effects.
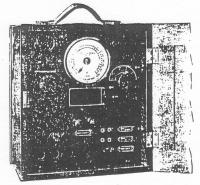
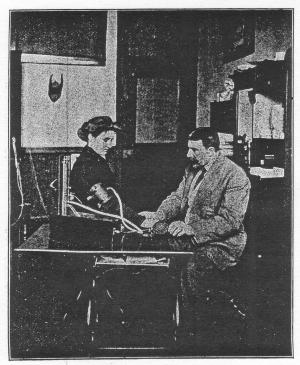
Taking the Blood Pressure. As a knowledge
of the patient’s blood pressure is vitally necessary to the physician using
high frequency currents it is important that he should have an instrument
for its rapid and accurate determination. The instrument used for
this purpose is called a sphygmomanometer and a number of satisfactory
machines are on the market. The diaphragm type is shown in Figs.
44 and 44b
The mercury type is shown in Fig. 44a. Its action
depends on opposing the pressure of a column of mercury with the pressure
of the blood in an artery. For this purpose the brachial artery,
in the arm above the elbow, is selected.
A cuff or band containing a rubber sack is fastened around
the arm above the elbow, with that part from which the rubber tube emerges
lying in front over the artery. Ordinarily the sleeve is rolled up
before the band is applied, but if the clothing is thin this is unnecessary.
A small rubber hose runs from the cuff to the machine, which has a U-shaped
tube containing mercury, with a gauge between. The zero mark on the
scale is placed on a level with the top of the mercury.
A rubber bulb is attached by a small tube to the machine,
and the physician holds this bulb in one hand, while with the other he
keeps a finger on the pulse in the patient’s wrist. The bulb is now
compressed and immediately air fills the cuff and the column of mercury
begins to rise. The operator continues to slowly inflate the cuff
until the pressure of the latter shuts off the blood in the brachial artery
and the pulse can no longer be felt at the wrist. When this occurs
the pressure of the column of mercury has balanced the pressure of the
blood in the artery and the reading on the scale opposite the top of the
column is the patient’s blood pressure.
In using the instrument it is customary to force the mercury
a little above the point where the pulse ceases to be felt and then wait
two or three seconds until the column settles to the point of the reappearance
of the pulse. By doing this one, two, or three times an absolutely
accurate reading may be depended on.
The scale reads from 0 to 300. The normal is 120.
The numbers refer to millimeters of mercury. A variation of 10 millimeters
up or down would not necessarily imply abnormal pressure, but 140 or more
would be presumptive of the presence of or tendency to arteriosclerosis.

Another instrument for accurately determining blood pressure
is the tycos diaphragm type of instrument, shown in Fig. 44.
This is not a mercury instrument, but the readings are
obtained by indirect, internal pressure on sensitive diaphragm chambers,
so sensitive indeed that every action of the heart is shown plainly by
the hand on the dial, as the hand works co-incidently with the heart.
With this instrument the observer can accurately determine
complete blood pressure, by that we mean maximal or systolic; minimal or
diastolic, and pulse pressure (the difference between the two). This
is not easy with a mercury instrument, because the great inertia of mercury
renders it difficult to obtain a diastolic pressure, for mercury requires
one and one-half seconds to recover itself, while in one second we have
had one and one-fourth heart impulses, so you can see that mercury does
not act quickly enough to accept the second impulse. Diastolic pressure
with a mercury machine may be obtained by the auscultatory method described
later on.
The minimal or diastolic pressure is fully as essential
as the maximal or systolic, for without an exact diastolic to subtract
from the systolic we cannot get the most important thing in blood pressure,
that is the pulse pressure, for by pulse pressure alone can it be determined
whether a pathological condition is compensated for or not.

The normal pulse pressure (difference between diastolic
and systolic) should be from 20 to 55 millimeters.
The determining of pulse pressure by those using the high
frequency current is absolutely essential, for, as said before, by this
we can tell whether a condition is compensated for, and whether the use
of high frequency current is indicated or contraindicated.
As an illustration, we will say that we have a case with
a systolic pressure of 170, and a diastolic pressure of 140. This
shows, by subtracting one from the other, that the pulse pressure is 30,
therefore normal. No matter then if the systolic be 170, for the
pulse pressure being normal shows that the condition is compensated (or
the pulse pressure could not be normal), and in these cases any further
reduction of systolic blood pressure must be accompanied by a corresponding
decrease in diastolic pressure or compensation will be interfered with.
Of course, if the systolic was reduced to 160 and the
diastolic remained 140, compensation would still exist, but would be at
its low limit, and the patient would probably not be as comfortable as
with 165 or 170, with 140 as the diastolic. If however, under auto-condensation
both systolic and diastolic pressures decreased, if not always the same
reduction, at least without the pulse pressure going below 20, the treatment
may be persisted in until the systolic pressure is normal.
Whenever the pulse pressure reaches 20 and stays there,
after carefully giving one to three additional treatments auto-condensation
should be abandoned. It has been carried as far as it can be of benefit
to the patient, no matter what the systolic pressure then may be, and I
would suggest spinal sparks to raise it slightly, that pulse pressure may
be at least 25.
Where the systolic reading is high it sometimes happens
that the pulse pressure will, when auto-condensation is employed, drop
to 20, or even 18, but after a few days the diastolic will reduce enough
to give an increased pulse pressure, and thereafter both systolic and diastolic
keep reducing in proportion, in which case the treatment is kept up.
See further discussion and examples under Arteriosclerosis, Chapter VIII.
There are two methods of determining blood pressure with
the tycos type, which I have taken from Dr. Cowing’s book, “Blood Pressure
Technique Simplified.”
First, the method of oscillation.
Place the bag over the arm with the two tubes well under
the arm and over the brachial artery. Wrap the remainder of the sleeve
around the arm much the same as you would apply a bandage, tucking at least
six inches of the sleeve under the last fold. Then place the sphygmomanometer
in one tube and the bulb in another and you are ready for reading.
Care should be taken not to put the sleeve on tight enough to cause any
apprehensive feeling in the patient. Place the fingers lightly over
the radial artery and send the pressure in the cuff up to the point where
the pulse disappears or is obliterated. This is the systolic or maximal
reading.
It is desirable that the patient’s wrist be supported
from below by the palm of the doctor’s hand, while the first and second
fingers lie with their tips over the artery. Thus the weight of the
hand is prevented from shutting off the pulse too soon.
Second, the method of auscultation. This is, by
far, the most practical method of accurately determining blood pressure,
as the dangers of personal equation are greatly lessened. See Fig.
44c.
Bare the arm, adjust the sleeve well up (as above described),
place the stethoscope over the brachial artery. Now gradually inflate
the bag, and the first and second sounds of the heart will become audible.
Increase the pressure in the bag to the point where all sounds cease.
At this point will be the exact systolic or maximal pressure.

Having obtained this, gradually release the air by means
of the valve, and the first and second sounds of the heart will become
apparent, increasing in volume as they approach the diastolic point, at
which point the second sound will entirely disappear.
The above method cannot be employed where aortic insufficiency
exists or where there is a dilatation of the vessels. These conditions
being observed, when the pressure is first increased on the brachial, as
soon as a slight pressure is placed on the artery, a pistol-shot tone is
heard, and will continue with but little variation throughout the observation.
When this condition exists it is absolutely necessary to resort to the
oscillatory method. It is also necessary to use the method by oscillation
when the pulse is feeble.
Having now accurately determined both systolic and diastolic
pressure, we compute the pulse pressure.
Pulse pressure is obtained by subtracting the diastolic
from the systolic, for example:
Systolic pressure, 120; diastolic pressure, 90; the difference,
pulse pressure, 30, and, as previously stated, it should not be less than
20, and would also indicate a pathological condition as probable if over
55.
In about 7,000 cases Cowing obtained the following average
normals:
Children from 10 to 17, 85 to 110 mm.
Adults from 21 to 40, 120 to 130 mm.
Adults from 40 to 50, 120 to 135 mm.
Adults from 50 to 60, 135 to 145 mm.
It is well to remember that there is an ever increasing
hardening of the arteries as one grows older, and a person of 65 or over
can very easily have a blood pressure of 160 and still be a comparatively
healthy individual. At the same time if these changes were not taking
place the blood pressure would remain the same, no matter what the age
of the patient might be. Female pressure is 10 mm. Lower than that
of males. Any blood pressures, however, between the ages of 21 and
50, lower than 100 or higher than 150,can safely be termed pathological
cases.
Leading life insurance companies now insist on the examiner
taking the blood pressure. Most of them reject applicants whose pressure
is 160 or higher, whether any other reason is apparent or not; just as
they do where the pulse is persistently above 90.
An easy method of keeping the range of blood pressure
in mind, which I have employed in my classes, is as follows:
Consider 120 the normal. At 20 above or below that
is 140 or 100, the warning signal is out, and at 20 more either way (160
or 80) the brink of the precipice has been reached and a pathological condition,
and probably a dangerous one, exists.
|
|
|
|
|
|
|
|
|
|
|
|